Baseline characteristics
In a cohort of 267,408 participants (median age 57 years, 50.31% female), adherence to recommended health behaviors was evaluated. Participants were categorized into three groups: high adherence group (meeting 5–6 criteria; n = 53,690, 20.08%), moderate adherence group (meeting 3–4 criteria; n = 158,023, 59.09%), and low adherence group (meeting 0–2 criteria; n = 55,695, 20.83%). Subsequent comparisons revealed that individuals in the high adherence group were more frequently female, more likely to reside in rural areas, to be employed, to achieve a university-level education or higher, to maintain a normal BMI, and to report higher household incomes compared to those in the low adherence group. Baseline characteristics of participants stratified by adherence to healthy lifestyle behaviors are summarized in Table 1.
Health lifestyle behaviors and digestive system diseases
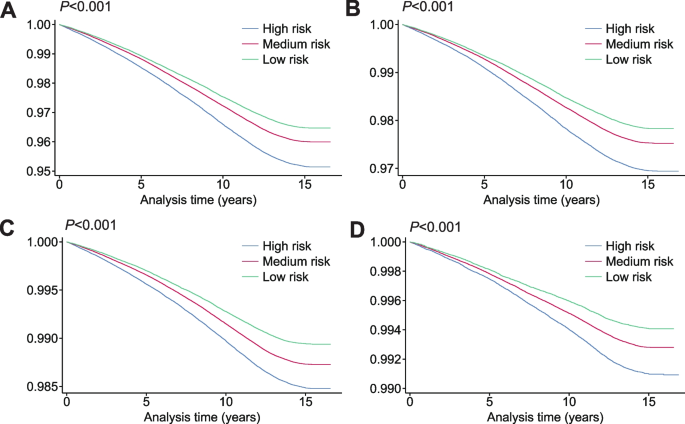
Survival analysis revealed a stepwise decrease in survival rates with increasing risk categories (Fig. 2). Participants in the low-risk class exhibited the highest survival probability, accompanied by the most gradual decline in the survival curve. The intermediate-risk class showed moderate survival outcomes, while the high-risk class was associated with the lowest survival rate and the most pronounced decline in the survival curve. Greater adherence to healthy lifestyle behaviors correlates with improved survival outcomes. This association corresponds to a lower cumulative incidence of overall digestive system diseases (Fig. 2A), including upper gastrointestinal (Fig. 2B), lower gastrointestinal (Fig. 2C), and hepatobiliary and pancreatic diseases (Fig. 2D). However, the downward trends observed in Fig. 2C and D appear minimal if not zero.
Survival curves for digestive system disease patients in different risk groups. A represents digestive system diseases, B represents upper gastrointestinal diseases, C represents lower gastrointestinal diseases, and D represents hepatobiliary and pancreatic diseases; All models adjusted for age, sex, ethnic background, BMI, residence, employment, education, and household income
A Cox proportional hazards model was employed to quantify the association between healthy lifestyle adherence and the risk of 20 digestive system diseases (Table 2). Notable variations in disease incidence emerged when participants were stratified by the number of healthy behaviors practiced. Upon adjusting for age, sex, ethnicity, BMI, residence, employment, education, and household income, an inverse relationship between healthy lifestyle adherence and disease risk was observed. In particular, compared with participants exhibiting low adherence, those with moderate adherence demonstrated an adjusted HR of 0.82 (95% CI: 0.80 to 0.84), while high adherence was associated with an adjusted HR of 0.72 (95% CI: 0.70 to 0.74).
Upper gastrointestinal diseases
Compared to the low adherence group, the high adherence group exhibited a lower incidence of upper gastrointestinal diseases (0.71, 95% CI: 0.68 to 0.73), including six diseases: gastroesophageal reflux (0.72, 95% CI: 0.69 to 0.75), esophageal cancer (0.41, 95% CI: 0.30 to 0.56), gastric ulcer (0.64, 95% CI: 0.57 to 0.72), duodenal ulcer (0.59, 95% CI: 0.50 to 0.69), gastritis and duodenitis (0.68, 95% CI: 0.65 to 0.72), and gastric cancer (0.54, 95% CI: 0.39 to 0.75). The moderate adherence group had also a lower incidence of upper gastrointestinal diseases (0.81, 95% CI: 0.79 to 0.83), including six diseases: gastroesophageal reflux (0.82, 95% CI: 0.79 to 0.84), esophageal cancer (0.73, 95% CI: 0.61 to 0.86), gastric ulcer (0.73, 95% CI: 0.67 to 0.79), duodenal ulcer (0.79, 95% CI: 0.71 to 0.88), gastritis and duodenitis (0.81, 95% CI: 0.78 to 0.83), and gastric cancer (0.62, 95% CI: 0.50 to 0.76). Notably, five of the six conditions in the high adherence group registered HR under 0.7, underscoring a substantial decline in risk. Even gastric cancer in the moderate adherence group showed a significant effect with an HR of 0.62 (95% CI: 0.50 to 0.76).
Lower gastrointestinal diseases
Compared to the low adherence group, the high adherence group exhibited a lower incidence of lower gastrointestinal diseases (0.70, 95% CI: 0.67 to 0.72), except for intestinal malabsorption (0.88, 95% CI: 0.74 to 1.05), including five diseases: irritable bowel syndrome (0.72, 95% CI: 0.66 to 0.79), ulcerative colitis (0.61, 95% CI: 0.51 to 0.74), Crohn’s disease (0.59, 95% CI: 0.46 to 0.76), diverticular disease (0.68, 95% CI: 0.66 to 0.71), and colorectal cancer (0.75, 95% CI: 0.68 to 0.84); The moderate adherence group also had a lower incidence of lower gastrointestinal diseases (0.83, 95% CI: 0.81 to 0.86), including six diseases: irritable bowel syndrome (0.83, 95% CI: 0.78 to 0.90), malabsorption (0.86, 95% CI: 0.74 to 0.99), ulcerative colitis (0.75, 95% CI: 0.66 to 0.85), Crohn’s disease (0.63, 95% CI: 0.52 to 0.75), diverticular disease (0.83, 95% CI: 0.80 to 0.85), and colorectal cancer (0.91, 95% CI: 0.84 to 0.98). Of note, ulcerative colitis, Crohn’s disease, and diverticular disease in the high adherence group demonstrated HR values below 0.7, reflecting a marked reduction in risk. Furthermore, Crohn’s disease in the moderate adherence group also exhibited a significant effect with an HR of 0.63 (95% CI: 0.52 to 0.75).
Hepatobiliary, pancreatic diseases and other diseases
Compared to the low adherence group, the high adherence group exhibited a lower incidence of hepatobiliary and pancreatic diseases (0.66, 95% CI: 0.62 to 0.70), including seven diseases: liver fibrosis and cirrhosis (0.37, 95% CI: 0.29 to 0.46), alcoholic liver disease (0.12, 95% CI: 0.08 to 0.18), liver cancer (0.69, 95% CI: 0.49 to 0.96), cholelithiasis (0.72, 95% CI: 0.67 to 0.77), cholecystitis (0.69, 95% CI: 0.59 to 0.81), acute pancreatitis (0.56, 95% CI: 0.47 to 0.67), and pancreatic cancer (0.70, 95% CI: 0.55 to 0.88). The moderate adherence group had a lower incidence of hepatobiliary and pancreatic diseases (0.80, 95% CI: 0.77 to 0.83), except for pancreatic cancer (0.94, 95% CI: 0.79 to 1.11), including six diseases: liver fibrosis and cirrhosis (0.58, 95% CI: 0.51 to 0.66), alcoholic liver disease (0.46, 95% CI: 0.40 to 0.53), liver cancer (0.62, 95% CI: 0.48 to 0.78), cholelithiasis (0.83, 95% CI: 0.79 to 0.88), cholecystitis (0.81, 95% CI: 0.73 to 0.90), and acute pancreatitis (0.73, 95% CI: 0.65 to 0.82). It is worth highlighting that the majority of conditions in the high adherence group exhibited a marked reduction in risk. Additionally, liver fibrosis and cirrhosis, alcoholic liver disease, and liver cancer in the moderate adherence group reached HR levels below 0.7, confirming a robust protective association. For the acute appendicitis, compared to the low adherence group, we observed that the adjusted HR for the high adherence group was significant (0.80, 95% CI: 0.68 to 0.94), while the moderate adherence group showed no significance (0.89, 95% CI: 0.78 to 1.00).
Multiple digestive system diseases
Compared to the low adherence group, participants in the moderate adherence group had significantly lower risks of developing multiple digestive system diseases (0.78, 95% CI: 0.76 to 0.80, P < 0.001), while those in the high adherence group had even lower risks (0.63, 95% CI: 0.60 to 0.65, P < 0.001). For upper gastrointestinal diseases, lower gastrointestinal diseases, and hepatobiliary and pancreatic diseases, the adjusted HRs for the moderate adherence group compared to the low adherence group were 0.77 (95% CI: 0.74 to 0.80), 0.78 (95% CI: 0.73 to 0.82), and 0.63 (95% CI: 0.58 to 0.69), respectively. For the high adherence group, the adjusted HRs were 0.63 (95% CI: 0.59 to 0.66), 0.62 (95% CI: 0.58 to 0.67), and 0.52 (95% CI: 0.46 to 0.59).
Separate analyses
To evaluate the impact of healthy lifestyle adherence on the incidence of digestive system diseases, Cox proportional hazards models were employed (Fig. 3). During the follow-up period, both the moderate (HR = 0.82, 95% CI: 0.80 to 0.84) and high adherence groups (HR = 0.72, 95% CI: 0.70 to 0.74) experienced significantly lower risks compared with the low adherence group, displaying a clear dose–response trend.
The relationship between each healthy behavior lifestyle and digestive system diseases. All models adjusted for age, sex, ethnic background, BMI, residence, employment, education, and household income. A represents digestive system diseases, B represents upper gastrointestinal diseases, C represents lower gastrointestinal diseases, and D represents hepatobiliary and pancreatic diseases
In analyses of individual healthy lifestyle behaviors, each behavior independently contributed to a reduced risk of digestive system diseases. Moderate alcohol consumption was associated with a HR of 0.98 (95% CI: 0.96 to 1.00, P = 0.046), while never smoking exhibited a stronger protective effect with a HR of 0.85 (95% CI: 0.83 to 0.86, P < 0.001). Adequate sleep duration was associated with a HR of 0.90 (95% CI: 0.88 to 0.91, P < 0.001), and regular physical activity showed a HR of 0.89 (95% CI: 0.87 to 0.91, P < 0.001). Similarly, adherence to a healthy diet and limited sedentary behavior reduced disease risk, with HRs of 0.93 (95% CI: 0.91 to 0.95, P < 0.001) and 0.90 (95% CI: 0.88 to 0.92, P < 0.001), respectively. These results highlight the independently protective effects of each behavior, reinforcing the importance of adopting multiple healthy lifestyle practices.
Further analyses examined the effects of healthy lifestyle behaviors on specific categories of digestive system diseases, including upper gastrointestinal diseases (Fig. 3B), lower gastrointestinal diseases (Fig. 3C), and hepatobiliary and pancreatic diseases (Fig. 3D). Consistent inverse associations were observed across all disease categories, indicating that all six healthy lifestyle behaviors exert protective effects across different types of digestive system diseases. Additionally, almost no interaction effects, whether synergistic or antagonistic, were observed among the six healthy lifestyle behaviors for any category of digestive system diseases. This indicates that the protective effects of these behaviors are additive and independent, suggesting that individuals can focus on increasing their adherence to as many healthy behaviors as possible without concern for optimizing specific combinations.
Sensitivity analyses
Sensitivity analyses supported the robustness of the main findings. Excluding participants whose digestive system disease diagnoses were solely based on self-report did not alter the conclusions, with adherence to a greater number of healthy lifestyle behaviors remaining significantly associated with lower risk of digestive system diseases (Additional file 1: Table S6). In sensitivity analysis considering no alcohol consumption as healthy drinking behavior, the estimates of the association were similar to the main analyses (Additional file 1: Table S7). Excluding participants with less than two years and five years of follow-up did not materially change the findings. This analysis further supported that the protective associations observed were unlikely to be influenced by early disease onset or reverse causation (Additional file 1: Table S8-S9). A 0–6 point score based on six lifestyle behaviors was developed and linearly validated. Results showed a significant linear association between cumulative healthy behaviors and reduced risk of digestive diseases, strengthening our main conclusions (Additional file 1: Table S10). Stratified analyses by sex, age, and study center (Additional file 1: Table S11), exclusion of participants lost to follow-up (Additional file 1: Table S12-S13), Bonferroni correction for multiple testing (Additional file 1: Table S14), and multiple imputation of missing covariates (Additional file 1: Table S15-S16) all yielded results consistent with the primary analysis. A higher number of adhered physical activity-related behaviors was generally associated with reduced risk of digestive system diseases, though nonsignificant for a few specific conditions (Additional file 1: Table S17). The subgroup analyses yielded consistent results across both BMI strata (BMI < 25 kg/m2 and ≥ 25 kg/m2), aligning with the primary findings. This consistency underscores the beneficial role of adhering to a greater number of healthy lifestyle factors in reducing the risk of digestive system diseases, irrespective of baseline BMI status (Additional file 1: Table S18).