Research Highlights:
- For people with Type 2 diabetes, following at least six healthy lifestyle habits when taking GLP-1 RA medications can lower their risk of heart attack, stroke, hospital visits due to cardiovascular disease and death, more than medication alone or healthy lifestyle changes alone.
- A study of more than 63,000 military veterans with Type 2 diabetes who took GLP-1 RA medications found that those with at least six healthy lifestyle habits had a 50% lower risk of serious cardiovascular events when compared to veterans with a lower adherence to a healthy lifestyle who were receiving standard diabetes care but not taking GLP-1 RA medication.
- Note: The study featured in this news release is a research abstract. Abstracts presented at American Heart Association’s scientific meetings are not peer-reviewed, and the findings are considered preliminary until published as full manuscripts in a peer-reviewed scientific journal.
Embargoed until 4 a.m. CT/5 a.m. ET, Monday, Nov. 3, 2025
DALLAS, Nov. 3, 2025 — People with Type 2 diabetes who combined healthy lifestyle habits with GLP-1 receptor agonist (GLP-1 RA) medications had a greater reduction in risk of major adverse cardiovascular events, including heart attack, stroke or cardiovascular disease death, compared to people only taking the medication, according to a preliminary study to be presented at the American Heart Association’s Scientific Sessions 2025. The meeting, Nov. 7-10, in New Orleans, is a premier global exchange of the latest scientific advancements, research and evidence-based clinical practice updates in cardiovascular science.
“Lifestyle modifications are recommended as the cornerstone for preventing and managing Type 2 diabetes,” said lead study author, Xuan-Mai Nguyen, M.D., Ph.D., a researcher with the Department of Veterans Affairs Boston Healthcare System and second-year medicine resident at the University of California, Los Angeles. “Our study’s findings suggest that people with Type 2 diabetes taking GLP-1 receptor agonists can improve their heart health even more by adding and maintaining healthy lifestyle habits. They also indicate that if someone does not have access to GLP-1 RAs, adopting healthy lifestyle habits can still lower the risk of having a stroke, heart attack or dying from heart-related issues.”
People living with Type 2 diabetes are twice as likely to die from cardiovascular disease, according to Know Diabetes by Heart – a collaborative initiative of the American Heart Association and the American Diabetes Association. The incidence of Type 2 diabetes has more than doubled in the past 20 years in the U.S.
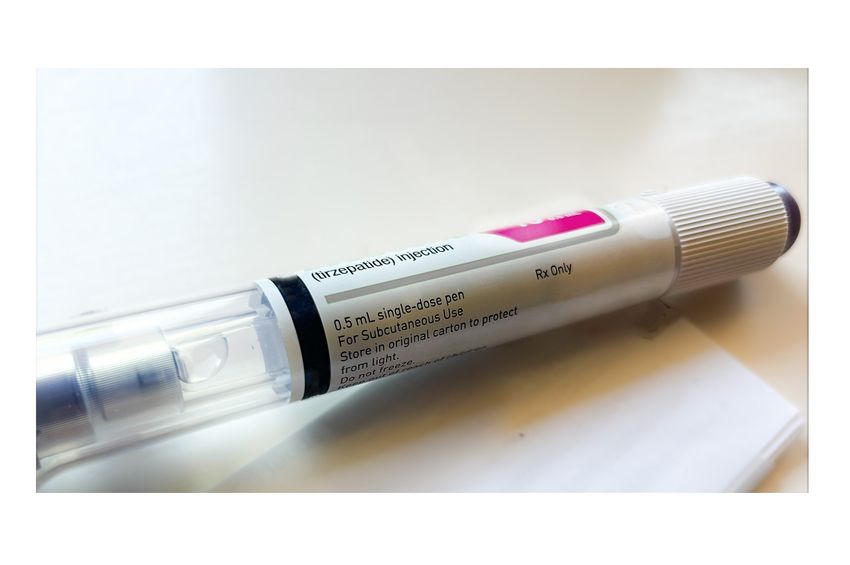
GLP-1 RA medications are injectable medications that lower blood sugar to treat diabetes, but also reduce appetite and can be used for weight loss. While research has proven the positive impact of the medications on heart health, and it is well known that healthy lifestyle factors can lead to a healthier heart, this study investigated how lifestyle factors influenced the association between GLP-1 RA medications and heart outcomes in people with Type 2 diabetes.
Researchers reviewed health information of people within the Million Veteran Program, a national program that studies how genes, lifestyle, military experiences and exposures affect health and wellness in U.S. veterans. The program uses data from medical records, biospecimens and self-reported surveys.
The study included data for more than 63,000 veterans who had Type 2 diabetes with no previous history of heart attack, stroke, cancer or advanced chronic kidney disease. Information was gathered on heart-healthy lifestyle habits, including healthy eating, physical activity, not smoking, restful sleep, no-to-moderate alcohol intake, good stress management, social connection and support and no opioid addiction. Researchers analyzed different combinations of lifestyle factors and medication use, with comparisons of people using GLP-1 RAs versus people not using this class of medication and also considered the number of protective lifestyle habits reported by each study participant.
Researchers then calculated each participant’s risk of major adverse cardiovascular events, which included non-fatal heart attacks, non-fatal strokes, death due to cardiac issues. When examined individually, all of the healthy lifestyle factors were independently associated with the participants having a lower likelihood of major adverse cardiovascular events.
The analysis also found:
- There was a 63% lower risk of a major cardiovascular event among participants adhering to all eight healthy lifestyle habits compared to those adhering to one or fewer.
- The risk of a major cardiovascular event was 20% lower among veterans taking GLP-1 RA medications, compared to those who did not use the medications, which is similar to what prior research has shown.
- There was a 50% reduction in risk of major cardiovascular events among people who took GLP-1 RA medications and who also adopted at least six healthy lifestyle habits. This was in comparison to participants who did not take a GLP-1 RA medication and only followed three or fewer healthy lifestyle habits.
“Taking a GLP-1 RA alone is less effective than combining it with other beneficial lifestyle factors. Achieving some healthy lifestyle behaviors can lower the risk of a major adverse cardiovascular event,” Nguyen said. “The more healthy lifestyle factors adopted, the better.”
Chiadi E. Ndumele, M.D., Ph.D., FAHA, chair of the American Heart Association’s Council on Lifestyle and Cardiometabolic Health, noted that “This is a very interesting study with powerful observations about the combined impact of healthy lifestyle and GLP-1 RA use on cardiovascular risk.
“It is important to keep in mind that a healthy lifestyle is often associated with confounding variables that could bias the results, such as other health behaviors or socioeconomic status. Hence, interpreting the findings should be done thoughtfully,” said Ndumele, who is the director of Obesity and Cardiometabolic Research at Johns Hopkins School of Medicine. “Nonetheless, these findings suggest that a healthy lifestyle really complements the powerful effects of GLP-1RAs. Rather than medications versus lifestyle, health care professionals should really be emphasizing both to achieve the best clinical outcomes for our patients.”
Study limitations include that the estimations were based on observational data; the study group primarily consisted of white male veterans, so the findings may not be applicable to a more diverse population; and the research does not predict how the rates of cardiovascular risk may change for adults without Type 2 diabetes who take GLP-1 RA medications to treat obesity.
Study details, background and design:
- The prospective cohort study included 63,656 adults with Type 2 diabetes within the Million Veteran Program with no previous history of heart attack, stroke, cancers or advanced chronic kidney disease. A total of 6,191 participants developed a major adverse cardiac event during the follow up period.
- About 6% of the participants were women; 82% were white veterans; about 13% were Black veterans and 4% were listed as other. About 8% were Hispanic veterans.
- The study included 418,513 person-years of follow-up – the cumulative number of years patients were tracked.
- Participants who adopted a higher number of positive lifestyle habits were more likely to be currently married, have a higher level of education and family income, and were less likely to have obesity and less likely to be Black.
- About 1 million veterans nationwide have joined the program since it launched in 2011.
- The study period was from 2011 to September 30, 2023.
Co-authors, disclosures and funding sources are listed in the abstract.
Statements and conclusions of studies that are presented at the American Heart Association’s scientific meetings are solely those of the study authors and do not necessarily reflect the Association’s policy or position. The Association makes no representation or guarantee as to their accuracy or reliability. Abstracts presented at the Association’s scientific meetings are not peer-reviewed, rather, they are curated by independent review panels and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting. The findings are considered preliminary until published as a full manuscript in a peer-reviewed scientific journal.
The Association receives more than 85% of its revenue from sources other than corporations. These sources include contributions from individuals, foundations and estates, as well as investment earnings and revenue from the sale of our educational materials. Corporations (including pharmaceutical, device manufacturers and other companies) also make donations to the Association. The Association has strict policies to prevent any donations from influencing its science content and policy positions. Overall financial information is available here.
Additional Resources:
###
About the American Heart Association
The American Heart Association is a relentless force for a world of longer, healthier lives. Dedicated to ensuring equitable health in all communities, the organization has been a leading source of health information for more than one hundred years. Supported by more than 35 million volunteers globally, we fund groundbreaking research, advocate for the public’s health, and provide critical resources to save and improve lives affected by cardiovascular disease and stroke. By driving breakthroughs and implementing proven solutions in science, policy, and care, we work tirelessly to advance health and transform lives every day. Connect with us on heart.org, Facebook, X or by calling 1-800-AHA-USA1.
For Media Inquiries and American Heart Association Expert Perspective: American Heart Association Communications & Media Relations:
Bridgette McNeil: Bridgette.McNeill@heart.org
For Public Inquiries: 1-800-AHA-USA1 (242-8721)
heart.org and stroke.org