Stay connected with The Oklahoman: How to subscribe online
Through our website, app, e-edition, newsletters, news alerts, social media and more, The Oklahoman is here for you. Here’s how to stay connected.
Adam’s Journal
Here’s a question from an Oklahoma Medical Research Foundation coworker:
I recently had my gallbladder removed, and pretty much every nurse I talked to at the hospital said they had, too. If this is part of a larger trend, why is this happening? And how can we function without this organ if it’s doing something important?
Dr. Scofield Prescribes
To understand what the gallbladder does, we have to start with the liver.
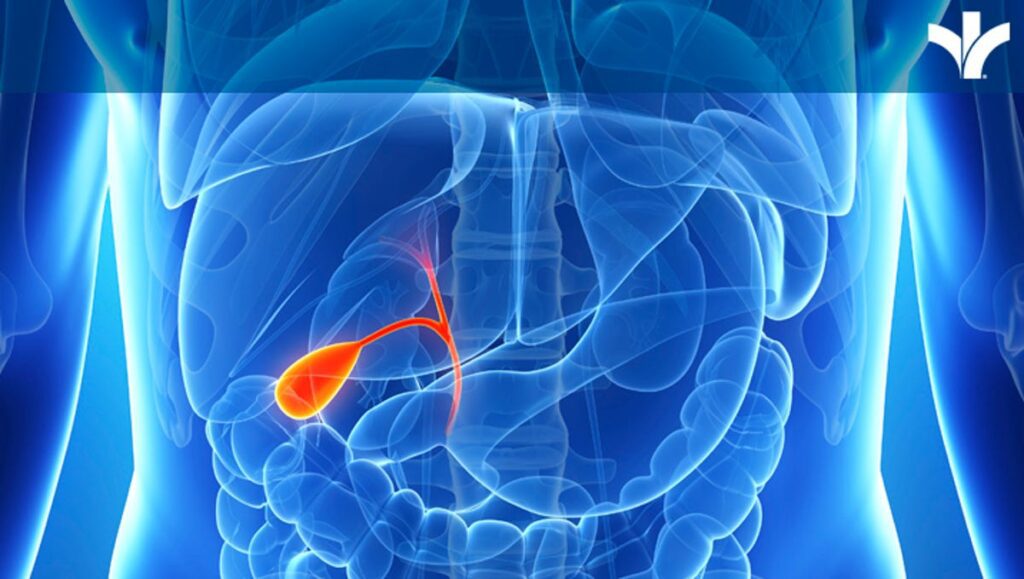
The liver makes bile, which plays a critical role in digesting fat. The gallbladder then stores bile, releasing it into the small intestine to aid digestion after fat is consumed.
When the gallbladder malfunctions — most often due to hard particles of bile, or gallstones, that form in the gallbladder — it causes symptoms like post-meal abdominal pain, nausea and vomiting. Although the typical course of treatment long involved a “cooling off” period of weeks or months before surgery to remove the gallbladder, evidence now shows that patients are best off having that surgery within 72 hours.
Gallbladder issues are a common problem, and they appear to be growing more so. In a U.S. National Health and Nutrition Examination Survey from 1988-1994, 6% of respondents reported a history of gallbladder surgery. When the same survey was given in 2017-2020, the figure had nearly doubled, with 11.5% of respondents reporting a history of gallbladder surgery.
What that means is that each year, more than a half million Americans have their gallbladders removed, with some sources placing the current figure as high as 1.2 million.
Like so many health trends, this one seems to be attributable to our diet and lifestyle. Specifically, the risk for gallbladder diseases increases with a variety of factors, including a fatty diet, a sedentary lifestyle, being overweight or obese, and having high blood pressure, high levels of body fat, increased blood sugar or diabetes.
As just about anyone knows, we’ve seen increases in all of these risk factors in recent years. So, it’s unsurprising that we’ve seen a corresponding uptick in gallbladder disease, which most often affects women and grows more common as we age.
Although the gallbladder aids in the digestion of fat, it’s not required. But when it’s removed, the body loses the ability to store the bile the liver produces. So, post-surgery, the liver continuously makes bile and releases it into the bloodstream.
This means that after gallbladder removal, patients may have trouble with high-fat meals, which can cause nausea, vomiting and diarrhea. However, this usually lessens after a few months, when patients learn what they can and cannot eat, and when they begin to regulate portions more strictly to control fat consumption.
Dr. Hal Scofield is a physician-scientist at the Oklahoma Medical Research Foundation, and he also serves as associate chief of staff for research at the Oklahoma City VA Medical Center. Adam Cohen is OMRF’s senior vice president and general counsel. Send your health questions to contact@omrf.org.