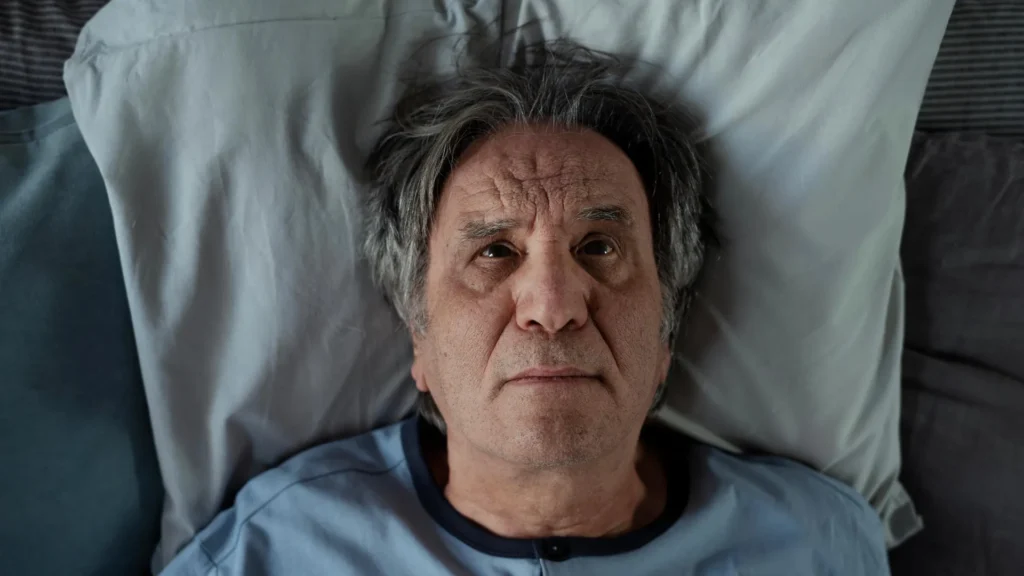
Alzheimer’s disease often throws a person’s daily patterns into disarray. Difficulty sleeping through the night, restless tossing, and frequent daytime naps are common early warning signs. In later stages, patients often experience “sundowning,” a period of increased confusion and agitation that tends to occur later in the day. These patterns hint at a close relationship between Alzheimer’s progression and the circadian system — the internal body clock that regulates sleep, wakefulness, and other daily biological cycles. Until recently, however, scientists did not fully understand how deeply this connection ran.
A team of researchers at Washington University School of Medicine in St. Louis has now demonstrated, in mouse models, that Alzheimer’s disease disrupts circadian rhythms within specific brain cells. This disturbance alters how and when hundreds of genes switch on and off, changing key processes that help the brain function properly.
Their findings, published October 23 in Nature Neuroscience, suggest that restoring or stabilizing these internal rhythms could open up a new approach to treating Alzheimer’s.
“There are 82 genes that have been associated with Alzheimer’s disease risk, and we found that the circadian rhythm is controlling the activity of about half of those,” said Erik S. Musiek, MD, PhD, the Charlotte & Paul Hagemann Professor of Neurology at WashU Medicine, who led the study. In mice engineered to model the disease, these genes no longer followed their usual daily patterns. “Knowing that a lot of these Alzheimer’s genes are being regulated by the circadian rhythm gives us the opportunity to find ways to identify therapeutic treatments to manipulate them and prevent the progression of the disease.”
The Burden of Sleep Disruption
Musiek, who co-directs the Center on Biological Rhythms and Sleep (COBRAS) at WashU Medicine and specializes in aging and dementia, noted that disturbed sleep is one of the most frequent problems reported by caregivers of Alzheimer’s patients. His earlier work showed that sleep changes begin years before memory loss becomes evident. Beyond exhaustion for both patients and caregivers, these disruptions create stress that may accelerate the disease’s progression.
Breaking this cycle, he said, starts with identifying where it begins. The body’s circadian system regulates roughly 20% of all genes in the human genome, orchestrating vital processes such as digestion, immune response, and sleep-wake cycles.
In earlier research, Musiek identified a protein called YKL-40 that naturally fluctuates throughout the day and helps control normal levels of amyloid in the brain. Too much YKL-40, which is linked to Alzheimer’s risk in humans, can trigger the build-up of amyloid — a sticky protein that forms plaques, one of the hallmarks of the disease.
Amyloid’s Effect on the Brain’s Timing Mechanisms
Because Alzheimer’s symptoms follow a repeating daily pattern, the team suspected more circadian-regulated proteins and genes might be involved. In the new study, they examined gene activity in the brains of mice that developed amyloid build-up, as well as in healthy young mice and older mice without plaques. Samples were collected every two hours over a full 24-hour period to track how gene expression changed across the circadian cycle.
The researchers found that amyloid deposits disrupted the normal rhythm of hundreds of genes in two key types of brain cells — microglia and astrocytes. Microglia act as the brain’s immune cells, clearing away waste and harmful materials, while astrocytes help neurons communicate and maintain healthy function. Many of the affected genes are normally responsible for microglia’s ability to remove waste, including amyloid.
Although these genes were not entirely switched off, their usual order and timing became chaotic, weakening the brain’s coordinated system for removing toxins.
New Rhythms and Potential Therapies
The study also revealed that amyloid plaques appeared to create new rhythmic patterns in genes that do not usually follow a daily cycle. Many of these genes are involved in inflammation or the brain’s response to stress and imbalance.
According to Musiek, these discoveries suggest that therapies aimed at adjusting circadian rhythms in microglia and astrocytes could support healthier brain activity.
“We have a lot of things we still need to understand, but where the rubber meets the road is trying to manipulate the clock in some way, make it stronger, make it weaker or turn it off in certain cell types,” he said. “Ultimately, we hope to learn how to optimize the circadian system to prevent amyloid accumulation and other aspects of Alzheimer’s disease.”
This research was supported by the National Institute on Aging (R01AG054517, T32AG058518), the National Institute of Neurological Disorders and Stroke (R01NS102272), and the National Institutes of Health (R00AG061231). The authors note that the content reflects their findings and does not necessarily represent the official view of the NIH.