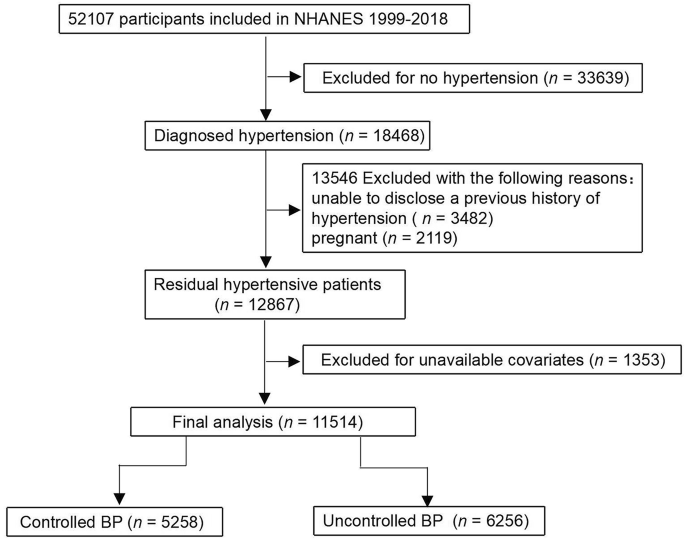
Table 1 summarizes the baseline characteristics of the study population. The mean age of participants was 50.66 ± 10.78 years, with 50.94% being male. Non-Hispanic Whites accounted for 39.54%, while 41.49% of participants were classified as low-income. A total of 47.64% had at associate degree (AA) or high education, and 44.04% were covered by private health insurance. The uncontrolled group had higher levels of LDL-C, HDL-C, TC, current smoking, current drinker, and sodium intake, while the controlled group showed higher BMI, fiber intake, and waist circumference. Additionally, the controlled group had a higher prevalence of MS, CHD, stroke, HF, and CKD compared to the uncontrolled group.
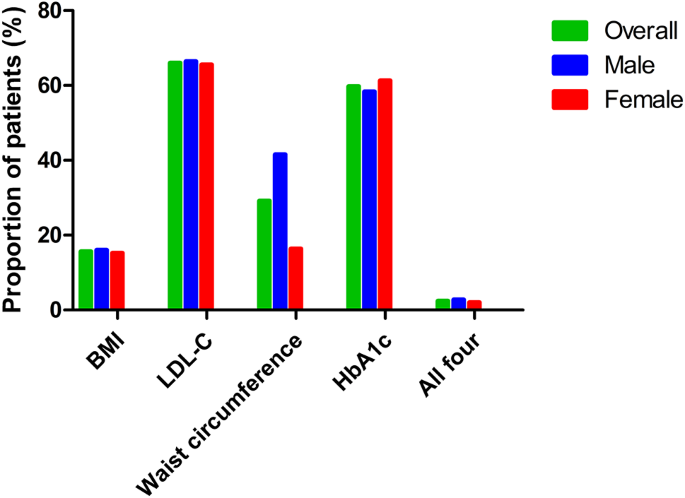
Table 2 shows that 15.62% of non-elderly hypertensive patients met the BMI target, with lower rates observed among Hispanics (10.86%) and those with AA or high education or above (14.48%). A total of 66.02% achieved the LDL-C target, while only 29.19% met the waist circumference goal. Lower attainment of the waist circumference goal was observed among women, non-Hispanic Whites, low-income individuals, and those with higher education. For HbA1c, 59.79% of participants met the target, with non-Hispanic Whites and higher-income groups showing higher success rates. Only 2.41% of patients achieved all four targets. Patients with public Medicare had better performance in meeting BMI, LDL-C, and HbA1c targets.
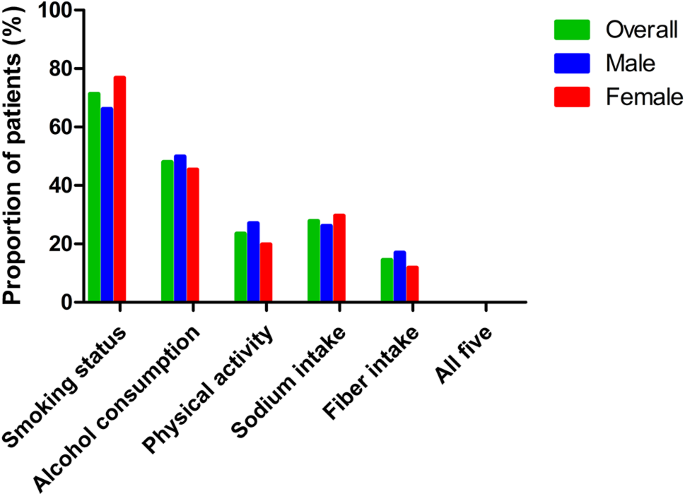
Table 3 shows that 71.32% of participants met the smoking target, with higher rates among women, Hispanics, high-income individuals, those with AA or high school education, and private insurance holders. The alcohol consumption target was achieved by 47.97%, with better outcomes among men, non-Hispanic Blacks, high-income individuals, those with higher education, and public Medicare recipients. The PA target was met by only 23.45%, with lower rates among women, non-Hispanic Blacks, those with lower education, and public Medicare holders. Sodium intake goals were achieved by 27.83%, with lower attainment among men, non-Hispanic Whites, those with AA or high education, high income, and private insurance. The dietary fiber target was met by 14.44%, with the lowest rates observed among women, low-income individuals, those with lower education, and public Medicare recipients. Only 0.03% of participants met all five lifestyle modification targets.
Table 4; Fig. 2 present the percentages [% (n)] of non-elderly hypertensive patients meeting recommended risk factor control targets, stratified by comorbidities. Achievement rates for BMI targets were lower among patients with MS, HF, and DM. Conversely, higher rates of LDL-C control were observed in patients with CHD, stroke, HF, DM, and CKD. Control of waist circumference was generally suboptimal across all comorbidity groups. HbA1c control was less frequent in MS patients but more prevalent in HF patients. The overall achievement rate for all four risk factor control targets was notably reduced among patients with MS and DM.
Bar chart showing the proportion of patients meeting individual risk factor targets (BMI, LDL-C, waist circumference, HbA1c) and all four targets, stratified by gender and overall. BMI, body mass index; LDL-C, low-density lipoprotein cholesterol. The “All four” indicator represents participants who simultaneously met all four individual lifestyle targets listed
Table 5; Fig. 3 present the percentages [% (n)] of non-elderly hypertensive patients achieving recommended lifestyle modification targets, categorized by comorbidities. A higher proportion of patients with MS and DM successfully met smoking cessation goals, while those with CHD, stroke, and HF exhibited lower success rates. Patients with CHD and CKD demonstrated higher success rates in achieving alcohol consumption goals. PA target adherence was consistently low across all comorbidity groups. Sodium intake goals were more frequently met by HF patients, whereas DM patients struggled with sodium restriction. Fiber intake goals were less frequently achieved among patients with stroke, HF, and CKD.
Bar graph showing the proportion of patients meeting lifestyle targets for smoking status, alcohol consumption, physical activity, sodium intake, fiber intake, and all five targets, categorized by gender and overall. The “All five” indicator represents participants who simultaneously met all five individual lifestyle targets listed
Table 6 presents the results of univariate logistic regression analyses for failing to meet risk factor control and lifestyle modification targets. The analysis indicates that being male, Hispanic, having a high school diploma or higher, and having comorbid MS or DM are associated with an increased risk of failing to control risk factors. Risks for not meeting lifestyle modification targets are associated with being male, non-Hispanic Black, low income, private insurance, public Medicare, and having comorbid stroke.
Table 7 presents the results of the multivariate logistic regression analysis. Compared with women, men had nearly twice the odds of failing to achieve risk factor control (OR 1.98, 95% CI 1.57–2.49, P < 0.0001). Participants with an AA or higher were also more likely to have uncontrolled risk factors compared to those with less than a high school education (OR 1.58, 95% CI 1.19–2.10, P = 0.002). Importantly, individuals with MS had a significantly higher risk of uncontrolled risk factors than those without MS, as indicated by an OR of 0.03 for the comparison “no vs. yes” (95% CI 0.02–0.03, P < 0.0001). Similarly, individuals with DM had greater odds of uncontrolled risk factors than those without (OR 0.47 for “no vs. yes”, 95% CI 0.34–0.65, P < 0.0001).
Table 8 presents the multivariate logistic regression results for poor adherence to recommended lifestyle modifications. Compared with women, men had a 36% higher likelihood of failing to meet lifestyle targets (OR 1.36, 95% CI 1.13–1.64, P = 0.001). Hispanic participants had a significantly lower risk of poor lifestyle adherence compared to non-Hispanic Whites (OR 0.57, 95% CI 0.46–0.71, P < 0.0001), suggesting better adherence in this subgroup. Participants with high socioeconomic status were significantly less likely to have poor lifestyle control than those with low socioeconomic status (OR 0.64, 95% CI 0.50–0.82, P = 0.0005), indicating a protective effect of higher socioeconomic status. In contrast, individuals covered by public Medicare insurance had more than twice the odds of failing to achieve lifestyle targets compared to those with private insurance (OR 2.54, 95% CI 1.38–4.66, P = 0.0003), highlighting a potential disparity based on insurance type.