This study revealed that nocturia is correlated with various sleep issues, including mid-wakefulness, difficulty falling asleep, and shallow sleep in the Japanese general population using an Internet survey. It also identified gender- and age-related characteristics in the relationship between nocturia and sleep issues. This study also highlighted that while some sleep-promoting habits are appropriately recognized, others may need to be reconsidered in the context of nocturia.
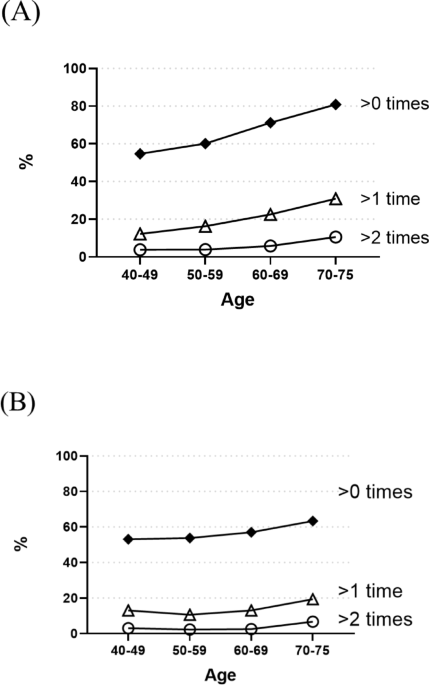
Regarding aging, this survey showed that the prevalence of nocturia increases with age, while the condition of sleep dissatisfaction decreases. This may be because individuals who have reached retirement age are relieved of work-related stress, and as their domestic responsibilities, such as childcare, gradually decrease, they are able to get the sleep they need23,24. However, among older adults (≥ 60 years), individuals with fewer nocturnal urinary frequency tend to be more satisfied with their sleep, whereas those with a higher frequency of nocturia tend to have lower overall sleep satisfaction. In other words, although sleep satisfaction generally increases with age, severe nocturia may interfere with it. An observational cross-sectional study of patients admitted to a urology department reported that sleep disorders were more common in patients with LUTS25, and another cohort study showed that men with nocturia were more likely to experience excessive daytime sleepiness26. These reports are consistent with our findings. Thus, there is a possibility that a significant number of patients with sleep issues may also require treatment for nocturia.
The same tendency was seen in younger adults (< 60 years), where a high percentage of participants with high nocturnal urinary frequency with dissatisfied with their sleep. However regardless of the nocturnal urinary frequency, the proportion of younger adults dissatisfied with their sleep was significantly higher. This suggests that factors other than nocturia contribute to sleep dissatisfaction in younger adults. Previous reports have identified several important risk factors for sleep issues, including obesity, unemployment, lack of a regular exercise routine, and mental stress27. Given that age and gender differences have also been reported, it is possible that factors other than nocturia play a major factor in sleep issues among younger adults.
Next, we examined the relationship between sleep issues and nocturia and found that mid-wakefulness was significantly correlated with nocturia in both genders. In addition, difficulty falling asleep was significantly associated with nocturia in men, whereas shallow sleep was significantly associated with nocturia in women. Although nocturia is a direct cause of mid-wakefulness, previous reports have suggested that the relationship between sleep issues and nocturia varies by gender28,29. As men age, they are more likely to develop urological diseases (such as benign prostatic hyperplasia), which are often accompanied by frequent nighttime urination. Exposure to light during nighttime urinations increases sympathetic nervous system activity and suppresses melatonin secretion. Previous studies have shown that melatonin not only promotes sleep and induces fatigue-like states but also ultimately leads to increased bladder capacity and decreased urine volume6,30. A reduced secretion of melatonin can make it more difficult to fall back asleep and may also affect the progression of nocturia. On the other hand, nocturia may also be indirectly associated with difficulty falling asleep. One possible explanation is that individuals who have experienced frequent nocturnal awakenings due to nocturia may develop anxiety or anticipatory arousal at bedtime, fearing repeated awakenings during the night. This may contribute to difficulty initiating sleep31. Conversely, it is also plausible that difficulty falling asleep itself contributes to increased nocturnal urine production. Prolonged wakefulness before sleep might reduce the secretion of antidiuretic hormone (ADH), leading to increased nocturnal urine volume and frequency32. In this sense, the relationship between nocturia and difficulty falling asleep may be bidirectional, and further studies are warranted to clarify the causal pathways. According to Kim et al., the age-related decline in sex hormones occurs more rapidly in women than in men33. These hormonal changes make women more prone to shallow sleep in middle age, which can lead to more frequent nocturia due to increased arousal34. Given these significant gender differences in sleep issues and nocturia, it is important to investigate the underlying causes separately for each gender and to implement proactive interventions for sleep issues associated with nocturia.
Nocturia and sleep issues may be improved by lifestyle modifications, which should be implemented prior to pharmacotherapy. Examples of beneficial lifestyle habits include minimizing fluid intake (especially caffeine and alcohol) at least 2 h before bedtime, limiting total fluid consumption to less than 2 L/day, emptying the bladder before going to bed, ensuring barrier-free access to a toilet, increasing exercise, reducing dietary salt intake, avoiding smoking, and achieving weight loss in overweight individuals17,19. Since beverages like coffee, which contain high levels of caffeine, can affect circadian rhythm and have diuretic effects, they should be avoided before bedtime18.
In this survey, we found that “Drinking tea or other sleep-inducing drinks” and “Drinking alcohol” were significantly more common among individuals with nocturia, regardless of gender. Notably, these habits were undertaken with the intention of promoting good sleep. However, consuming fluids before bedtime is unsuitable for those with nocturia, and drinking alcohol can adversely affect not only nocturia but also sleep quality. These findings provide valuable insights into the type of education that should be offered to the general population with sleep disorders and nocturia. In addition, “Not drinking too much water” was also significantly more common among those with nocturia. It is generally accepted that limiting fluid intake is an effective countermeasure for improving nocturia, and in some cases, physicians may advise patients to reduce their fluid consumption. This is thought to be the result of individuals with nocturia being aware that limiting fluid intake may help alleviate their symptoms and consciously making an effort to do so. This approach is generally appropriate for individuals whose nocturia is primally caused polyuria/nocturnal polyuria. However, indiscriminate fluid restriction carries the risk of heat-related illnesses, such as heatstroke. Therefore, it is essential to provide guidance on maintaining an appropriate level of fluid intake based on urine output (20–30 mL/kg body weight/day)35.A higher proportion of individuals in the group with nocturia and satisfied sleep reported engaging in moderate daytime exercise compared to those with unsatisfied sleep. Although no causal relationship can be inferred from these findings, this observation may suggest that certain daytime lifestyle factors, such as exercise, are associated with perceived sleep satisfaction in individuals with nocturia.
A multivariable analysis examining the correlation between nocturia (≥ 2 vs. <2 episodes) and various lifestyle habits, adjusted by age, lifestyle habits, and sleep satisfaction, suggested that using good bedding may be associated with a reduced risk of nocturia. In a previous study evaluating the effects of bedding materials on sleep quality, it was found that sleeping with a high rebound mattress topper induced a marked decline in core body temperature during the initial phase of nocturnal sleep, and this decline was associated with an increase in deep sleep. Furthermore, the study suggested that reduced muscle activity required for rolling over is another factor that improves sleep quality36. In addition, previous literature in sleep medicine suggests that bedding and sleepwear can influence sleep quality by affecting thermal comfort. For example, a systematic review by Xinzhu Li et al. reported that optimal bedding varies depending on the population and environmental conditions37. Wool bedding and sleepwear may promote faster sleep onset and deeper sleep in cooler conditions, especially among older individuals and those with sleep difficulties. In contrast, cotton sleepwear may be more suitable for healthy young adults under moderate temperatures. While our study cannot determine causality, nor specify the types of bedding used, it is possible that using bedding appropriate to individual needs and environmental conditions may contribute to improved sleep quality, and thereby indirectly help alleviate nocturia.
A strength of the present study was its large population size, which enabled age-stratified and sex-separated analyses. These analyses provided a clear understanding of the relationships among nocturia, sleep issues and lifestyle habits, and suggested that taking effective countermeasures tailored to each sleep issue may help to improve nocturia. However, several limitations must be acknowledged. First, there is a possibility of selection bias among survey participants. This survey was limited to individuals with internet access and those who participated in online surveys, many of whom may have had a particular interest in sleep issues. Nevertheless, the distribution of the participants across regions closely matched the national population ratio (Chi-square 2.121, df 7, p = 0.950) (Fig. S1). Although Internet surveys are highly anonymous and adherence to self-reported behaviors may be uncertain, large-scale nationwide epidemiological surveys have already been successfully conducted both in Japan and other countries38,39. We lacked clinical information on background factors for participants. The causes of nocturia are diverse, and lower urinary tract symptoms such as benign prostatic hyperplasia and overactive bladder, as well as internal diseases such as heart failure and diabetes, have a significant impact on the frequency of urination. In addition, drugs that have a diuretic effect, antipsychotic drugs, and steroids that affect sleep and wakefulness have a significant impact on nocturia and the degree of sleep and wakefulness. Further research that includes background factors such as these underlying diseases and medications would strengthen the present findings. Finally, as this is a cross-sectional study, it is difficult to determine the directionality of the relationship between nocturia and sleep issues. In the future, prospective cohort studies or interventional trials would be valuable for further advancing our understanding of this relationship.
In summary, the severity of nocturia was significantly correlated with lower sleep satisfaction and various sleep issues. Our findings also suggest that some individuals with nocturia may have misconceptions about which lifestyle habits promote good sleep. These insights could prove useful in guiding sleep hygiene modifications and in developing educational strategies for individuals with nocturia and sleep issues.